Joint Replacement Surgery: A Guide for Patients in Lahore
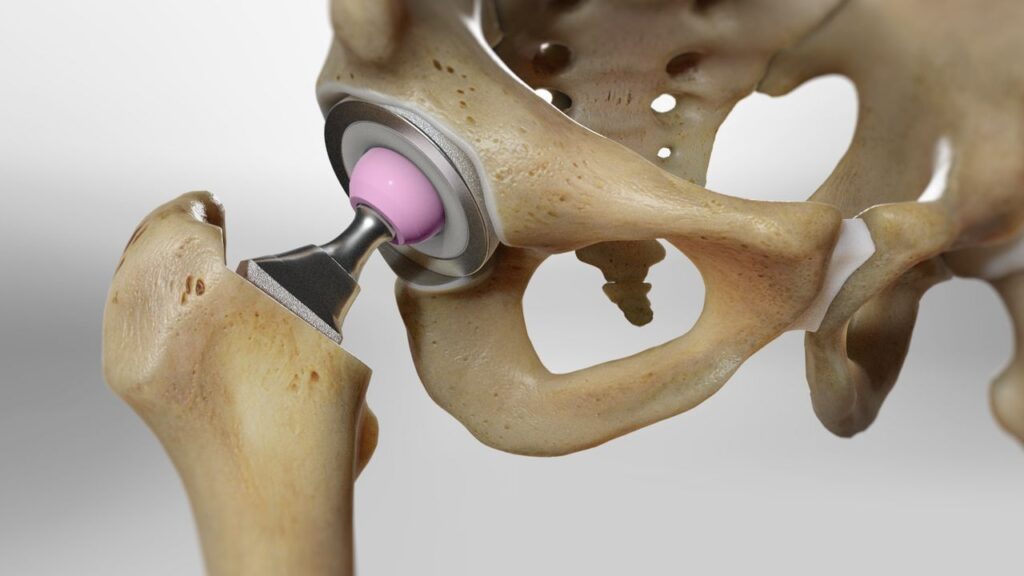
Joint replacement surgery is a life-changing procedure for many patients in Lahore suffering from chronic pain and limitations due to severe arthritis or joint damage. Here at Dr. Waqas Javed’s Orthopedic Surgery practice, we understand the significant decision you face when considering joint replacement. This guide aims to answer your questions and empower you to make informed choices about your healthcare. What is Joint Replacement Surgery? Joint replacement surgery involves replacing a worn-out or damaged joint with an artificial implant (prosthesis) made of metal, plastic, or ceramic. The prosthesis is designed to replicate the movement and function of a healthy joint, alleviating pain and improving mobility. Common joints replaced include hip, knee, shoulder, and ankle. Benefits of Joint Replacement Surgery Pain Relief: The primary benefit is significant pain reduction, allowing you to resume activities you previously enjoyed. Improved Mobility: Increased range of motion and flexibility lead to a more active lifestyle. Enhanced Quality of Life: Reduced pain and increased mobility can significantly improve your daily life. Durability: Modern prosthetics are designed to last for many years, with minimal limitations. Types of Joint Replacement Surgery Hip Replacement: Replaces the ball and socket joint of the hip. Knee Replacement: Replaces the worn surfaces of the knee joint. Shoulder Replacement: Replaces the damaged parts of the shoulder joint. Ankle Replacement: Replaces the bones and cartilage of the ankle joint (a less common procedure). Before Surgery Consultation: Dr. Javed will discuss your medical history, symptoms, and expectations to determine if joint replacement is the right option. Imaging Tests: X-rays, CT scans, or MRIs provide detailed images of the joint to plan the surgery. Physical Therapy: Pre-operative physical therapy strengthens the muscles surrounding the joint, aiding in post-surgical recovery. Medical Optimization: Addressing any underlying health conditions is crucial for a successful surgery. During Surgery Joint replacement surgery is typically performed under general anesthesia. Minimally invasive techniques, when possible, promote faster recovery. The damaged joint surfaces are removed and replaced with the prosthesis. After Surgery Pain Management: Medications will be administered to control pain. Physical Therapy: Post-surgical rehabilitation is crucial to regain strength, flexibility, and range of motion. Recovery Time: The recovery period varies depending on the joint replaced and your individual case. Dr. Javed will create a personalized rehabilitation plan to guide your recovery journey. Risks and Complications As with any surgery, there are potential risks associated with joint replacement, such as infection, bleeding, blood clots, and nerve damage. Dr. Javed will discuss these risks in detail during your consultation. Living with a Replaced Joint Modern prosthetics are highly durable, but certain activities may need modification. Dr. Javed will advise you on maintaining a healthy lifestyle and maximizing the longevity of your implant. Conclusion Joint replacement surgery can be a transformative procedure, offering significant pain relief and improved mobility. If you’re experiencing chronic joint pain and limitations in Lahore, Dr. Waqas Javed can guide you through the process and determine if joint replacement is the right solution for you. Schedule a consultation today to discuss your individual needs and explore the possibilities of a pain-free, active future.
Understanding Fractures: Types, Treatments, and the Road to Recovery

Fractures, or broken bones, are a common occurrence, affecting people of all ages and activity levels. Whether caused by a fall, a car accident, a sports injury, or even overuse, a fracture can be a painful and disruptive experience. However, understanding the different types of fractures, treatment options, and the recovery process can empower you to navigate this experience with confidence. This article serves as a comprehensive guide to fractures, providing you with the information you need to make informed decisions about your health. The Broken Landscape: Exploring Different Types of Fractures Fractures can be classified in various ways, depending on the severity, location, and appearance on an x-ray. Here’s a breakdown of some common types: Closed Fracture (Simple Fracture): The broken bone doesn’t pierce the skin. This is the most common type of fracture. Open Fracture (Compound Fracture): The broken bone breaks through the skin, creating a wound and increasing the risk of infection. Comminuted Fracture: The bone is shattered into multiple pieces. Displaced Fracture: The broken bone ends are misaligned. Non-displaced Fracture: The broken bone ends remain aligned. Stress Fracture: A small crack in the bone caused by repetitive stress, often seen in athletes. Understanding the Cause: Why Bones Break Several factors can contribute to a fracture: Trauma: A sudden impact from a fall, accident, or sports injury is a common cause of fractures. Overuse: Repetitive stress on a bone, particularly in athletes, can lead to stress fractures. Underlying Medical Conditions: Diseases like osteoporosis that weaken bones can increase the risk of fractures even from minor impacts. Recognizing the Signs: Symptoms of a Fracture A fracture can manifest through various symptoms: Pain: The most common symptom is pain at the fracture site, often worsening with movement. Swelling: Inflammation and swelling around the injured area are common. Bruising: Discoloration of the skin surrounding the fracture may occur. Deformity: In some cases, the affected limb may appear visibly deformed or bent at an unnatural angle. Loss of Function: Difficulty moving or putting weight on the injured limb is a common symptom. Seeking Help: Diagnosis and Treatment Options If you suspect a fracture, seek immediate medical attention. Here’s what to expect: Physical Examination: A doctor will examine the injured area, checking for pain, swelling, and deformity. Imaging Tests: X-rays are typically used to visualize the fracture and determine its location and severity. In some cases, additional imaging tests like CT scans or MRIs might be needed. Treatment Options: The best treatment for a fracture depends on the type and severity of the injury. Here are some common approaches: Immobilization: For minor fractures, casting or splinting may be sufficient to hold the broken bone fragments in place while they heal. Reduction: If the bone fragments are misaligned, a doctor might need to manually reposition them (closed reduction) or perform surgery (open reduction) to achieve proper alignment. Fixation: Once the bones are aligned, various methods may be used to hold them in place during healing. This can involve casts, splints, screws, plates, or rods. The Road to Recovery: Healing and Rehabilitation The recovery time for a fracture varies depending on the severity of the injury, your age, and overall health. However, a typical recovery timeline can look like this: Immobilization: The initial period involves wearing a cast or splint for several weeks to allow the bone fragments to heal. Physical Therapy: Rehabilitation exercises play a crucial role in regaining strength, flexibility, and range of motion in the injured area. Gradual Return to Activity: With your doctor’s guidance, you’ll gradually increase your activity level to return to your daily routine and desired activities. Preventing Fractures: Building a Strong Foundation While fractures can happen, there are steps you can take to minimize your risk: Maintain Bone Health: Eat a balanced diet rich in calcium and vitamin D, essential nutrients for strong bones. Weight-Bearing Exercise: Regular weight-bearing exercises like walking, running, or dancing help build and maintain bone density. Fall Prevention: For seniors or individuals with balance issues, taking steps to prevent falls is crucial. This includes installing grab bars in bathrooms, improving home lighting, and wearing proper footwear. Strength Training: Building strong muscles around your bones helps provide support and stability, reducing the risk of fractures during falls or injuries. Know Your Limits: Engage in activities appropriate for your age and fitness level. Pushing yourself too hard in sports or exercise can increase your risk of overuse injuries. Proper Equipment: Use appropriate safety gear for activities like cycling, skateboarding, or skiing to minimize the impact of falls. Living with a Fracture: Managing Pain and Promoting Healing While healing a fracture can be a frustrating wait, some strategies can help manage pain and promote recovery: Pain Management: Your doctor might prescribe pain medication to manage discomfort during the initial stages of healing. Over-the-counter pain relievers like ibuprofen or acetaminophen can also be helpful. Elevation: Elevating the injured limb above the heart level can help reduce swelling and pain. Ice Therapy: Applying ice packs to the injured area for short intervals (15-20 minutes at a time) can help reduce pain and inflammation. Healthy Diet: Eating a nutritious diet rich in fruits, vegetables, and whole grains provides your body with the essential nutrients it needs for healing. Patience and Optimism: Healing takes time. Be patient with your body and remain optimistic about a full recovery. Beyond the Basics: Complications and Long-Term Effects In some cases, complications can arise from fractures: Nonunion: The bone fragments fail to heal properly, leaving a gap between them. Malunion: The bone heals in an abnormal position, which can affect function and mobility. Infection: Open fractures are more susceptible to infection, requiring prompt medical attention and antibiotics. When to Seek Additional Help: If you experience any of the following symptoms after a fracture, consult your doctor immediately: Increased pain or swelling Numbness or tingling in the injured area Fever or chills (signs of infection) Difficulty moving the injured limb even after the cast or splint is removed Conclusion: Building Resilience and Moving
The Importance of Bone Health Throughout Life: Building a Strong Foundation
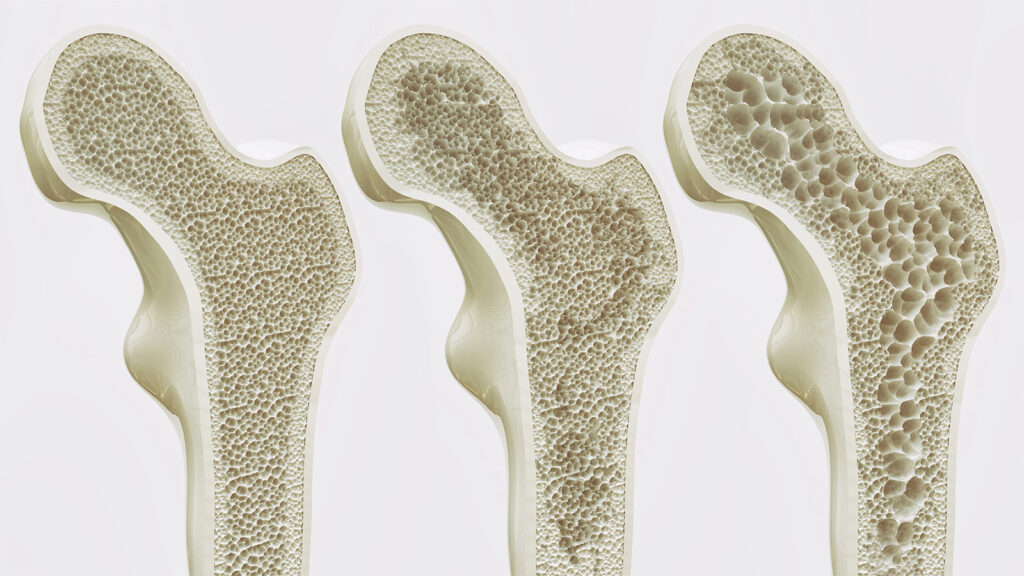
Our bones are more than just a rigid framework; they’re a living, dynamic tissue that plays a vital role in our overall health and well-being. From providing structure and support to our bodies to protecting vital organs and storing essential minerals, strong bones are the foundation of a healthy life. However, bone health is often overlooked until problems arise, like fractures or the debilitating condition osteoporosis. This article explores the significance of bone health throughout life, highlighting the key factors that contribute to strong bones at every stage. We’ll delve into the essential nutrients your body needs, explore the benefits of weight-bearing exercises, and equip you with knowledge to prevent osteoporosis and safeguard your skeletal system for years to come. Understanding Bone: A Dynamic Tissue Contrary to popular belief, bones are not static structures. They are constantly undergoing a remodeling process, with new bone formation occurring alongside the breakdown of old bone. This process is influenced by various factors, including diet, exercise, hormones, and even genetics. During childhood and adolescence, bone formation outpaces breakdown, leading to peak bone mass around the age of 30. After this peak, bone loss becomes a natural part of the aging process. However, the choices we make throughout life significantly impact the rate of bone loss and our risk of developing bone diseases. Building Strong Bones From the Start: Childhood and Adolescence The foundation for strong bones is laid early in life. During childhood and adolescence, when peak bone mass is being established, ensuring proper nutrition and adequate physical activity is crucial. Here’s how to nurture strong bones in your young ones: Nutrient Powerhouse: A balanced diet rich in calcium, vitamin D, and other essential nutrients is vital for bone development. Include plenty of calcium-rich foods like milk, yogurt, cheese, dark leafy greens, and fortified foods in their diet. Vitamin D helps the body absorb calcium, so ensure your child gets adequate sunlight exposure or consider vitamin D supplements if needed. Move It or Lose It: Encourage regular physical activity in children. Weight-bearing exercises like running, jumping rope, and playing sports stimulate bone growth and improve bone density. Maintaining Bone Health: Adulthood and Beyond While peak bone mass is reached by early adulthood, maintaining bone health throughout life is essential. Here are some key strategies for adults and seniors: Nutritional Support: Calcium and vitamin D remain crucial nutrients for bone health throughout adulthood. Continue incorporating calcium-rich foods and consider supplements if dietary intake is insufficient. Maintaining a healthy weight is also important, as excess weight puts additional stress on your joints. The Power of Weight-Bearing Exercise: Regular weight-bearing exercises are still vital for maintaining bone density and strength. Activities like walking, jogging, dancing, and stair climbing can significantly benefit bone health. Strength training exercises that target major muscle groups can also help improve bone health by strengthening the muscles surrounding the bones. Hormonal Considerations: Bone loss can accelerate in women after menopause due to declining estrogen levels. If you’re experiencing menopause, talk to your doctor about ways to manage bone loss, which might include hormone replacement therapy or medications specifically for bone health. Lifestyle Habits: Smoking and excessive alcohol consumption can negatively impact bone health. Quitting smoking and limiting alcohol intake are crucial steps towards maintaining strong bones. Preventing Osteoporosis: A Lifelong Commitment Osteoporosis, a condition characterized by low bone density and increased fracture risk, is a significant concern, particularly for older adults. While there is no cure for osteoporosis, several steps can be taken to prevent its development and manage its progression: Early Diagnosis and Intervention: Regular bone density scans, especially after the age of 50, can help identify bone loss early on. Early diagnosis allows for timely intervention and treatment to prevent fractures. Medication: Several medications are available to treat and prevent osteoporosis. Talk to your doctor about the best treatment options for your individual needs. Fall Prevention: Falls are a major cause of fractures in individuals with osteoporosis. Implementing fall prevention strategies, such as improving home safety and maintaining good balance through exercise, can significantly reduce fracture risk. Building a Strong Foundation for a Healthy Life By prioritizing bone health throughout life, you can significantly reduce your risk of fractures, improve your mobility and independence, and maintain an active lifestyle well into your golden years. Remember, it’s never too late to start taking care of your bones. Here’s a summary of key takeaways: Focus on a balanced diet rich in calcium, vitamin D, and other essential nutrients. Engage in regular weight-bearing exercises and strength training. Maintain a healthy weight. Limit alcohol consumption and quit smoking. Schedule regular bone density scans after the age of 50, especially for women after menopause. Talk to your doctor: Discuss your individual risk factors for bone loss and osteoporosis with your doctor. They can create a personalized plan to optimize your bone health and prevent future complications. Beyond the Basics: Additional Strategies for Optimal Bone Health While the core principles of bone health remain constant, here are some additional considerations that can further enhance your skeletal well-being: The Protein Factor: Protein plays a crucial role in bone health. Include lean protein sources like fish, chicken, beans, and lentils in your diet. Vitamin K and Bone Health: Emerging research suggests Vitamin K, particularly Vitamin K2, may play a role in bone health. Consider including foods rich in Vitamin K2 like leafy green vegetables, natto (fermented soybeans), and grass-fed dairy products in your diet. The Sunshine Vitamin: While sunlight exposure provides essential Vitamin D, excessive sun exposure can be harmful. Aim for moderate sun exposure without burning and consider vitamin D supplements if needed, especially during winter months or if you have limited sun exposure. Rest and Relaxation: Adequate sleep is essential for overall health, including bone health. Aim for 7-8 hours of quality sleep each night. Mind-Body Connection: Stress can negatively impact bone health. Techniques like meditation, yoga, and deep breathing can help manage stress and promote overall well-being. Building Strong Bones Together: Community and Support Maintaining
Arthritis: Embracing Life Despite the Pain

Arthritis, a condition characterized by inflammation and degeneration of joints, casts a long shadow over millions of people worldwide. It’s a leading cause of disability, significantly impacting daily activities and overall well-being. While there’s no cure, there are effective management strategies that can empower you to live an active and fulfilling life, even with arthritis. Understanding the Enemy: Different Types of Arthritis Knowing the specific type of arthritis you have is crucial for effective management. Here’s a breakdown of some common types: Osteoarthritis: The most prevalent type, osteoarthritis is caused by the wear-and-tear of the cartilage that cushions your joints. It typically affects weight-bearing joints like knees, hips, and spine, causing pain, stiffness, and swelling. Rheumatoid Arthritis: An autoimmune disease, rheumatoid arthritis attacks the synovial membrane, the lining of the joints. It can affect multiple joints, including hands, wrists, knees, and feet, leading to pain, inflammation, and joint deformity. Gout: This sudden and intense joint pain arises from a buildup of uric acid crystals in the joints, often affecting the big toe. Psoriatic Arthritis: Associated with the skin condition psoriasis, psoriatic arthritis can cause pain, swelling, and stiffness in joints, along with characteristic skin lesions. The Silent Thief: Recognizing the Signs of Arthritis Early diagnosis and intervention are key to managing arthritis effectively. Here are some common symptoms to watch out for: Joint Pain: A dull ache or sharp pain in the affected joint, often worsening with activity and improving with rest. Stiffness: A feeling of tightness or restricted movement in the joint, particularly noticeable after periods of inactivity. Swelling: Inflammation around the joint, causing visible puffiness. Redness: The affected joint may appear red and warm to the touch in some cases. Reduced Range of Motion: Difficulty bending or straightening the affected joint. Joint Deformity: In advanced stages, some types of arthritis can cause visible joint deformity. Empowering Yourself: Management Strategies for a Pain-Free Life While there’s no magic bullet for arthritis, a combination of strategies can significantly improve your quality of life: Medication: Different types of medications can help manage pain, inflammation, and disease progression. Consult your doctor to determine the best medication for your specific type of arthritis. Physical Therapy: A physical therapist can design a personalized exercise program to improve strength, flexibility, and range of motion in the affected joints. Exercise helps maintain joint health and reduces pain. Lifestyle Modifications: Maintaining a healthy weight reduces stress on your joints. A balanced diet rich in fruits, vegetables, and whole grains provides essential nutrients for joint health. Consider incorporating anti-inflammatory foods like fish and omega-3 fatty acids into your diet. Heat and Cold Therapy: Applying heat (heating pad) or cold (ice pack) to the affected joint can help relieve pain and inflammation. Assistive Devices: Using canes, walkers, or braces can provide support and stability, reducing stress on the joints and improving your ability to perform daily activities. Complementary Therapies: Exploring Additional Options Some people find relief with complementary therapies alongside conventional treatment. These can include: Acupuncture: This traditional Chinese medicine practice involves inserting thin needles into specific points on the body to alleviate pain. Massage Therapy: Massage can help relax muscles, improve circulation, and reduce pain. Yoga and Tai Chi: These gentle exercise forms promote flexibility, balance, and mindfulness, which can be beneficial for managing arthritis. The Road Ahead: Living Well with Arthritis Arthritis may be a chronic condition, but it doesn’t have to define your life. By understanding your condition, working with your doctor to develop a personalized management plan, and adopting healthy lifestyle habits, you can effectively manage your pain and maintain an active and fulfilling life. Remember, a positive attitude and perseverance are essential tools in your journey towards living well with arthritis.
Preventing Sports Injuries: Staying Active and Healthy in Lahore

For athletes of all ages in Lahore, participating in sports offers a multitude of benefits. From building teamwork and discipline to improving physical fitness and mental well-being, sports play a vital role in a healthy lifestyle. However, the thrill of competition and the push to excel can sometimes lead to unforeseen consequences – sports injuries. These injuries can range from minor muscle strains to debilitating ligament tears, forcing athletes to take a break from their beloved activities. Dr. Waqas Javed, a leading orthopedic surgeon in Lahore, emphasizes the importance of injury prevention for athletes of all levels. By incorporating simple yet effective strategies into your training routine, you can significantly reduce your risk of injuries and stay active for years to come. Understanding the Landscape: Common Sports Injuries Before diving into preventive measures, let’s explore some frequently encountered sports injuries: Overuse Injuries: These occur due to repetitive stress on muscles, tendons, and joints. Examples include runner’s knee (patellar tendinitis), swimmer’s shoulder (rotator cuff tendinitis), and shin splints. Acute Injuries: These are sudden injuries caused by a specific event, such as a fall, forceful impact, or awkward landing. Sprains (ligament tears), strains (muscle tears), and fractures fall under this category. Non-traumatic Injuries: These can be caused by improper technique, poor flexibility, or underlying medical conditions. Bursitis (inflammation of the fluid-filled sacs around joints) and stress fractures are examples. Building a Strong Foundation: Preventing Sports Injuries The good news is that many sports injuries are preventable. Here are Dr. Waqas Javed’s key recommendations for athletes in Lahore: Warm-up and Cool-down Religiously: Warm-up: Before any physical activity, dedicate 5-10 minutes to a dynamic warm-up that gradually increases your heart rate and blood flow. This can include light jogging, jumping jacks, lunges, arm circles, and leg swings. Cool-down: After your workout or game, spend another 5-10 minutes on static stretches to improve flexibility and reduce muscle soreness. Hold each stretch for 15-30 seconds and repeat 2-3 times. Strength Training is Your Ally: Building strong muscles around your joints provides better stability and support, reducing the risk of injuries. Work with a qualified trainer to develop a strength training program tailored to your specific sport and fitness level. Focus on exercises that target major muscle groups in your legs, core, and upper body. Listen to Your Body: Don’t push yourself through pain. Pain is often a signal from your body that something is wrong. Take rest days when needed, and gradually increase the intensity and duration of your workouts to avoid overtraining. Proper Technique is Paramount: Many injuries occur due to improper technique during training or competition. Invest in proper coaching or attend clinics to learn the correct form for exercises and movements specific to your sport. A trained coach can identify and correct any flaws in your technique that might put you at greater risk of injury. The Right Gear Matters: Wearing appropriate footwear and protective gear significantly reduces your risk of injuries. Invest in good quality shoes with proper arch support specific to your sport. Use protective gear like helmets, pads, and mouth guards as recommended for your sport. Maintain Flexibility: Regularly incorporate static stretches into your routine to improve flexibility and range of motion. This allows for better performance and reduces the risk of muscle strains and tears. Fuel Your Body Right: A balanced diet rich in essential nutrients provides your body with the building blocks it needs to perform at its best and recover from workouts. Include plenty of fruits, vegetables, whole grains, and lean protein in your diet. Stay hydrated by drinking plenty of water throughout the day, especially before, during, and after exercise. Listen to Your Limits: Don’t try to do too much too soon, especially if you’re new to a sport. Gradually increase the intensity and duration of your workouts to allow your body to adapt and build strength. Don’t be afraid to ask for help from a coach or trainer if you have any questions or concerns. Beyond Prevention: Recognizing and Managing Injuries Despite taking precautions, injuries can still occur. Here’s what to do if you experience a sports injury: Stop Immediately: The moment you feel pain, stop the activity immediately. Continuing to play on an injured body can worsen the injury and increase healing time. RICE Protocol: Apply the RICE protocol (Rest, Ice, Compression, Elevation) to reduce swelling and inflammation. Rest the injured area for at least 24-48 hours, apply ice packs for 15-20 minutes at a time (wrapped in a towel to prevent skin irritation. Building a Strong Foundation: Preventing Sports Injuries (continued) Cross-Training for Versatility: While focusing on your primary sport is important, incorporating cross-training activities into your routine can help prevent overuse injuries and improve overall fitness. Cross-training involves activities that work different muscle groups than your main sport. For example, a runner might incorporate swimming or cycling for low-impact cardio, while a basketball player could benefit from yoga or Pilates for core strengthening and flexibility. Recovery is Key: Don’t underestimate the importance of proper recovery. Allow your body adequate rest and recovery time between workouts and games. Schedule rest days and prioritize quality sleep (7-8 hours per night for adults) to allow your muscles to repair and rebuild. Consider incorporating activities like yoga or foam rolling to promote blood flow and muscle recovery. Listen to Your Coach or Trainer: A qualified coach or trainer can be a valuable asset in your injury prevention journey. They can assess your strengths and weaknesses, develop a personalized training program, and provide guidance on proper technique. They can also monitor your progress and adjust your training plan as needed to minimize your risk of injuries. Mental Toughness Matters: Mental strength plays a crucial role in injury prevention. Athletes who are mentally focused and disciplined are less likely to make mistakes that can lead to injuries. Practice mindfulness techniques like meditation or deep breathing to stay focused and in control during training and competition. Building mental resilience will also help you manage pain and persevere through
Understanding Knee Pain: Causes, Treatments, and Getting Back on Your Feet

Knee pain is a relentless foe, plaguing people of all ages and activity levels. It can transform simple tasks like climbing stairs or walking into a daunting challenge. This article delves into the various culprits behind knee pain, explores potential treatment options, and equips you with knowledge to get back on your feet comfortably. Unveiling the Culprits: A Deep Dive into Knee Pain Causes Injury Arsenal: Sprains, strains, and tears involving ligaments, tendons, or cartilage can inflict knee pain. These injuries are often inflicted by sudden twists, falls, or repetitive stress. Ligament Tears: The ligaments act as stabilizers for your knee joint. A sprain signifies a mild tear, while a complete tear can significantly compromise joint stability and require medical attention. Tendon Trouble: Tendons connect muscles to bones. Tendinitis, the inflammation of a tendon, often occurs around the kneecap (patellar tendinitis) due to overuse. Cartilage Catastrophe: Cartilage cushions the bones within your knee joint. Tears or degeneration of cartilage can cause significant pain and grinding sensations. Arthritis Onslaught: This degenerative condition involves inflammation and breakdown of the joint’s cartilage. Osteoarthritis: The most common type, osteoarthritis is linked to aging and wear-and-tear. It can cause pain, stiffness, and swelling in the knee. Rheumatoid Arthritis: An autoimmune disease that attacks the joints, rheumatoid arthritis can affect multiple joints, including the knees, causing pain, inflammation, and joint deformity. Overuse Injuries: Repetitive activities like running, jumping, or squatting can overload your knee joint, leading to conditions like: Patellar Tendinitis: Inflammation of the kneecap tendon, often seen in runners and jumpers. Bursitis: Inflammation of the fluid-filled sacs cushioning the knee joint, like prepatellar bursitis (kneecap) or pes anserine bursitis (inner knee). Iliotibial Band Syndrome (ITBS): Inflammation of the IT band, a tissue on the outer thigh that runs down to the shinbone, causing pain on the outer side of the knee. Beyond the Usual Suspects: Alignment problems, baker’s cysts (fluid-filled pockets behind the knee), infections, and even weight gain can contribute to knee pain. Combating Knee Pain: A Multi-Pronged Approach to Relief The good news is that many knee pain cases respond well to conservative treatment, avoiding surgery. Here’s a breakdown of some effective non-surgical approaches: RICE Therapy: Rest, Ice, Compression, and Elevation are the pillars of initial pain management. Rest allows healing, ice reduces inflammation, compression minimizes swelling, and elevation improves circulation. Medication: Over-the-counter pain relievers like ibuprofen can help manage pain and inflammation. In some cases, stronger medications or injections may be prescribed by a doctor. Physical Therapy Powerhouse: Strengthening exercises for the muscles surrounding the knee improve stability and function. Physical therapists can also guide you through stretches to enhance flexibility and range of motion. This can help improve your posture and mechanics, reducing stress on the knee joint. Weight Management Matters: Maintaining a healthy weight reduces stress on your knee joints. Losing even a few pounds can significantly improve knee pain. When Surgery Takes Center Stage While non-surgical options are often successful, some cases necessitate surgical intervention. Here are some instances where surgery might be recommended: Conservative Treatment Roadblock: If conservative treatment fails to provide adequate relief after a reasonable trial period of several weeks or months. Severe Injuries: In cases of severe ligament tears, particularly those involving the ACL (anterior cruciate ligament), or complex fractures, surgery might be necessary to restore stability and function to the knee. Cartilage Concerns: When significant cartilage damage necessitates repair or replacement. Techniques like arthroscopy (minimally invasive surgery) can be used for cartilage repair, while knee replacements may be considered for severe arthritis. Prevention is Key: Keeping Your Knees Happy and Healthy By incorporating these tips into your routine, you can significantly reduce your risk of knee pain: Maintain a healthy weight. Warm up before exercise and cool down afterward. This helps prepare your muscles and joints for activity and reduces the risk of injury. Choose low-impact exercises like swimming or cycling. These activities provide a great workout without putting excessive stress on your knees. Invest in proper footwear with good arch support. Proper footwear can help maintain proper alignment and absorb shock during activities. Strengthen the muscles around your knees. Strong quadriceps, hamstrings, and calves can improve knee stability and function.
Pediatric Orthopedics: Addressing Common Childhood Bone and Joint Issues

Introduction Pediatric orthopedics is a crucial branch of medicine that focuses on the diagnosis and treatment of musculoskeletal issues in children. Unlike adults, children have unique physiological characteristics as their bodies are still growing, which necessitates a specialized approach to their bone and joint health. This article aims to shed light on common orthopedic issues in children and how they are addressed. Growth and Development Considerations The foundation of pediatric orthopedics lies in understanding the growth patterns and development of children’s bones, joints, and muscles. Since these structures are still developing, they respond differently to injury and disease compared to adults. For instance, the presence of growth plates (areas of growing tissue near the ends of long bones) in children can affect both the diagnosis and treatment of fractures and other conditions. Common Pediatric Orthopedic Conditions Several conditions are particularly common in the pediatric population: Developmental Dysplasia of the Hip (DDH): DDH is a condition where the hip joint does not develop properly, leading to a range of issues from mild instability to dislocation. Early diagnosis is critical for effective treatment, which may include bracing or surgery. Clubfoot: This congenital condition causes a newborn’s foot to be twisted or positioned at an odd angle. Treatment usually involves casting or bracing to gradually correct the foot position. Scoliosis: A condition characterized by an abnormal curvature of the spine. Management depends on the severity of the curve and can range from observation to bracing or surgery. Osgood-Schlatter Disease: A common cause of knee pain in growing adolescents, this condition is related to the inflammation of the area just below the knee where the tendon from the kneecap attaches to the shinbone. Diagnosis and Treatment Diagnosing pediatric orthopedic conditions often involves a combination of physical examination, medical history, and imaging tests such as X-rays, MRI, or ultrasound. Treatment strategies vary greatly depending on the condition and its severity, ranging from non-invasive methods like physical therapy and orthotic devices to surgical interventions in more severe cases. The Role of Pediatric Orthopedists Pediatric orthopedists play a vital role not just in treating existing conditions, but also in monitoring the child’s growth and development to prevent potential future issues. They work closely with families to provide education and guidance on managing and treating orthopedic conditions in children. Conclusion Pediatric orthopedics is a vital field that addresses the unique bone and joint health challenges faced by children. Through early diagnosis, appropriate intervention, and continuous monitoring, pediatric orthopedists help children lead healthy, active lives. Understanding these common conditions and their treatments empowers parents and caregivers to seek timely medical attention, ensuring the best possible outcomes for their children’s musculoskeletal health.
Dealing with Osteoarthritis: Pain Management and Lifestyle Modifications

Introduction Osteoarthritis, often referred to as OA, is the most common form of arthritis, affecting millions of people worldwide. It occurs when the protective cartilage that cushions the ends of the bones wears down over time. While osteoarthritis can damage any joint, the disorder most commonly affects joints in the hands, knees, hips, and spine. Managing osteoarthritis pain and adapting lifestyle changes are critical for improving quality of life for those affected. Understanding Osteoarthritis Osteoarthritis is a degenerative joint disease characterized by the breakdown of joint cartilage and underlying bone. Its symptoms often develop slowly and worsen over time and can include pain, stiffness, swelling, and decreased range of motion. While age is a significant risk factor, other factors like obesity, joint injuries, genetics, and occupations demanding repetitive joint movements also contribute to its development. Pain Management Strategies Medications: Over-the-counter pain relievers like acetaminophen, ibuprofen, and naproxen sodium can help ease osteoarthritis pain. For more severe pain, doctors may recommend prescription medications. Physical Therapy: A physical therapist can demonstrate exercises to strengthen the muscles around your joint, increase your flexibility, and reduce pain. Injections: In some cases, corticosteroid or hyaluronic acid injections are used to relieve pain. Alternative Therapies: Acupuncture, tai chi, and yoga can also help manage pain and improve function. Lifestyle Modifications Exercise: Regular movement helps maintain flexibility in the joints. Weight-bearing exercises like walking and swimming can be particularly beneficial. Weight Management: Excess weight adds additional stress to weight-bearing joints, such as the hips and knees. Losing weight can help reduce pain and prevent further joint damage. Heat and Cold Therapies: Applying heat or cold to the affected joints can relieve pain and reduce inflammation. Assistive Devices: Using devices such as canes, shoe inserts, braces, and splints can help in stabilizing weakened joints. Dietary Considerations A healthy diet rich in antioxidants, such as fruits and vegetables, can help reduce inflammation. Foods rich in omega-3 fatty acids, like salmon and flaxseeds, are also beneficial. Conclusion Living with osteoarthritis requires a multifaceted approach that combines medical treatments with lifestyle modifications. Staying active, managing weight, and employing various pain management techniques can significantly improve the symptoms of OA. Regular check-ups and communication with healthcare providers are essential in effectively managing this condition.
Understanding Carpal Tunnel Syndrome: Causes, Symptoms, and Treatment

Introduction Carpal Tunnel Syndrome (CTS) is a common condition that affects the hand and wrist, causing pain, numbness, and tingling. It occurs when the median nerve, which runs from the forearm into the palm of the hand, becomes pressed or squeezed at the wrist. This article aims to provide a comprehensive understanding of the causes, symptoms, and treatment options for Carpal Tunnel Syndrome. What is Carpal Tunnel Syndrome? The carpal tunnel is a narrow passageway on the palm side of your wrist, consisting of bones and ligaments. The median nerve, which controls sensations to the palm side of the thumb and fingers (except the little finger), and the tendons that bend the fingers, pass through this tunnel. CTS develops when swelling or irritation narrows this tunnel and causes the median nerve to be compressed. Causes of Carpal Tunnel Syndrome The exact cause of CTS is often difficult to identify, but it’s typically related to a combination of factors. These may include: Repetitive motions, like typing or any motions of the wrist that you do over and over, especially when your hands are lower than your wrists. Conditions such as hypothyroidism, obesity, rheumatoid arthritis, and diabetes. Pregnancy, due to hormonal changes and fluid retention. Genetic predisposition – some people have a smaller carpal tunnel. Symptoms of Carpal Tunnel Syndrome Symptoms usually start gradually and can include: Numbness, tingling, and pain in the hand and arm. A burning sensation in the fingers. Weakness in the hands and a tendency to drop objects. Symptoms often occur in both hands, but each hand can be affected differently. Diagnosis of Carpal Tunnel Syndrome Diagnosing CTS involves a review of medical history, a physical examination, and possibly some tests. These tests might include nerve conduction studies and electromyography to measure the electrical activity of muscles and nerves. Treatment Options for Carpal Tunnel Syndrome Treatment for CTS should begin as early as possible. Options include: Non-Surgical Treatments: Wrist splinting: A splint that holds your wrist still while you sleep can help relieve nighttime symptoms. Nonsteroidal anti-inflammatory drugs (NSAIDs): Medications such as ibuprofen may help relieve pain. Changes in daily activities: Identifying and modifying the activities that worsen your symptoms. Physical therapy: Exercises to stretch and strengthen the muscles in the hand and arm. Surgical Treatments: Carpal tunnel release surgery: A procedure to relieve pressure by cutting the ligament pressing on the median nerve. The surgery may be performed with traditional open surgery or with a smaller incision and a tiny camera to guide the surgeon. Lifestyle and Home Remedies Certain lifestyle changes and home remedies can also help relieve CTS symptoms. These include: Taking frequent breaks to rest hands. Avoiding activities that worsen symptoms. Applying cold packs to reduce occasional swelling. Conclusion Carpal Tunnel Syndrome is a condition that can significantly impact daily activities and quality of life. Understanding the causes and symptoms is the first step toward managing this condition. With appropriate treatment, including lifestyle changes, medical intervention, and possibly surgery, many people with CTS can find relief from their symptoms and return to their normal activities.
Duverney Fracture: Understanding this Rare Pelvic Injury

Introduction A Duverney fracture, although relatively uncommon, is an important type of pelvic injury that medical professionals, particularly those in emergency and orthopedic fields, should be aware of. This fracture involves a break in the iliac wing, one of the large, flat bones that form the pelvis. The nature of this fracture often leads to distinct clinical presentations and treatment considerations. What is a Duverney Fracture? A Duverney fracture specifically refers to an isolated fracture of the iliac wing, which is part of the pelvic bone. Unlike other pelvic fractures that often result from high-impact trauma and are associated with significant morbidity and mortality, Duverney fractures are typically caused by less severe trauma. They are often the result of a direct blow to the region, such as a fall onto the hip. Clinical Presentation and Diagnosis Patients with a Duverney fracture usually present with localized pain over the iliac crest, which may be exacerbated by certain movements or pressure. Unlike more severe pelvic fractures, Duverney fractures typically do not disrupt the pelvic ring and therefore, do not present with the instability or life-threatening complications seen in other types of pelvic fractures. Diagnosis is primarily made through radiographic imaging. Plain radiographs, such as pelvic X-rays, are typically sufficient to identify the fracture. However, in some cases, CT scans may be necessary to fully evaluate the extent of the injury. Treatment and Management The management of Duverney fractures primarily involves conservative treatment. This includes pain management, limited weight-bearing activities as tolerated, and possibly physical therapy. Surgical intervention is rarely required unless the fracture is significantly displaced or involves other complications. Recovery and Prognosis The prognosis for Duverney fractures is generally favorable, with most patients achieving full recovery. The key to successful recovery includes adequate pain management and appropriate physical rehabilitation to restore mobility and strength. Conclusion Duverney fractures, while less common than other types of pelvic fractures, present a unique clinical scenario. Their generally benign nature and favorable prognosis, when compared to other pelvic injuries, make them noteworthy in the context of trauma and orthopedic medicine. Awareness and proper management of this type of fracture are essential for optimizing patient outcomes.