Hemorrhage in the knee joint

Hemorrhage into the knee joint is called hemarthrosis. It manifests itself as pain, swelling, decreased mobility and changes in the contours of the joint. Blood from the knee must be evacuated, and this requires a puncture of the joint. Subsequently, the underlying disease that caused the hemorrhage is treated. Causes of hemorrhage into the joint cavity Depending on the cause of occurrence, knee hemorrhages are divided into three groups: Traumatic. Non-traumatic. Postoperative. The most common type of bleeding into the joint cavity is traumatic hemarthrosis. For blood to leak into the joint in significant quantities, serious tissue damage must occur: cartilage, bones or ligaments. Therefore, bleeding into the joint is a sign of severe trauma that may require surgical intervention: Up to 70% of all knee bleeds in adults are due to anterior cruciate ligament (ACL) rupture. In 10% of cases, the cause of hemorrhage is a meniscus tear. In 2-5%, hemorrhage is caused by a torn cartilage fragment or an intra-articular bone fracture. In 5% of cases, the cause is a rupture of the posterior cruciate ligament or knee joint capsule. In children, the leading cause is lateral patellar dislocation. Non-traumatic hemorrhage is usually associated with a blood clotting disorder, such as hemophilia, vitamin K deficiency, liver cirrhosis, and anticoagulant use. Rare causes of non-traumatic hemorrhage in the knee joint include diabetic arthropathy, vitamin C deficiency, septic arthritis, tumors in the knee area, hemangiomas, as well as ruptures of the arteries of the knee joint due to osteoarthrosis and degenerative changes in the posterior horn of the medial meniscus. Postoperative hemorrhages are most often associated with endoprosthetics. Less often, it develops as a complication of other knee surgeries. Symptoms After an injury, the joint swells over several hours. Mobility is significantly reduced, but the pain is not always severe. The pain can range from mild to severe, depending on the nature of the injury, and usually increases as blood accumulates inside the joint due to the pressure it exerts. All other symptoms depend on the type of injury. For example, when the meniscus is torn, the knee joint is blocked: a person cannot straighten, or less often bend, the leg. When the anterior cruciate ligament is torn, a feeling of instability appears in the knee, and during a clinical examination, the doctor can determine a positive anterior drawer symptom: the shin is excessively displaced forward during passive movement, since the tibia is no longer held by the torn ligament. Diagnostics Using ultrasound, you can see fluid in the knee, but you cannot reliably determine that it is blood and not inflammatory exudate. The most accurate method is considered to be MRI. With this procedure, it is possible to distinguish blood from other fluids, as well as to establish the cause of the hemorrhage, for example, to visualize torn ligaments or menisci. When intra-articular bone fractures are suspected, which account for only a small proportion of knee hemorrhage cases, radiography and CT scanning are the preferred diagnostic options. Treatment of hemorrhage in the knee joint Patients with hemarthrosis require a puncture of the knee joint. The doctor performs this procedure under local anesthesia. The doctor inserts a needle into the joint cavity to evacuate the accumulated fluid and inject medications into the knee. This procedure quickly reduces pain and improves knee mobility by reducing intra-articular pressure. The color of the fluid that the doctor obtains from the knee can help the doctor guess the cause of the hemorrhage. It can be pink, red, or brown, and in severe trauma it may contain fatty droplets. Other methods of conservative treatment: ice; anti-inflammatory drugs; immobilization; compression bandages. During the recovery period, massage, exercise therapy, and physical therapy are used. Some patients will need surgery to partially remove the meniscus or reconstruct the anterior cruciate ligament. At Dr. Waqas Javed’s Clinic, all knee interventions are performed using a minimally invasive arthroscopic method. Possible complications Severe or recurrent hemarthrosis can lead to destruction of intra-articular cartilage and osteoarthritis. The toxic effect of blood on the articular membrane causes its hypertrophy (proliferation) and fibrosis (scarring). Most often, complications develop with bleeding into a joint against the background of hemophilia, but this is a rare cause, accounting for no more than 1% of cases, and is mainly diagnosed at the age of 2-3 years. Repeated episodes of bleeding into the joint cavity can cause arthropathy with impaired joint mobility and patient disability. This complication develops in 20% of patients with hemophilia. In addition to the knee, other joints are also affected. Rehabilitation and exercise therapy After surgery or a period of immobilization, patients require rehabilitation. How long it will take depends on the nature of the injury. If after meniscus resection recovery takes only one and a half months, then after a rupture of the anterior cruciate ligament and its reconstruction, recovery takes six months. The main means of rehabilitation is considered to be therapeutic exercise, but other procedures are additionally used, such as massage, physiotherapy, mechanotherapy, electromyostimulation. Forecast After a knee puncture, the pain goes away in a few days, and most other symptoms disappear completely in a few weeks, unless there are gross anatomical defects in the knee. If there are such defects, then without treatment, a person will suffer from joint instability or recurrent blockades. Inflammatory processes (reactive synovitis) will worsen, and in the long term, the risk of osteoarthritis increases. Surgical treatment may be required to prevent these consequences. Prevention Prevention of knee hemorrhages is identical to injury prevention. It is necessary to warm up before training, exercise in good shoes, and avoid running on slippery surfaces. Unfortunately, there are no measures that will protect against knee injury with a 100% guarantee. If you notice that your knee is swollen, painful, and difficult to move as a result of an injury, contact Dr. Waqas Javed’s Clinic in Lahore. We will conduct diagnostics and find out whether there is blood in the joint or not. If there is, we will
Nutrition and diet for joint disease

There are many joint diseases, and for most pathologies, diet does not affect the clinical course, outcome, or effectiveness of treatment. But there are a few exceptions. For example, gout. With this disease, uric acid metabolism is disrupted, so a diet with limited purines is an important part of treatment. For most other diseases, the main goal of nutrition is to maintain normal weight or reduce excess weight. Let’s figure out what you can and cannot eat with some joint problems. The purpose of diet for diseases of the musculoskeletal system A diet for diseases of the musculoskeletal system can be aimed at: Providing bone and cartilage tissue with all the necessary substances so as not to disrupt metabolic processes. Prevent substances from entering the body that can worsen the condition of joints due to certain diseases. Maintain a normal weight or reduce excess weight to reduce the load on the sore joints of the lower extremities, primarily the knee and hip. It is worth noting that for most orthopedic diseases no diet is needed. Principles of proper nutrition for joint diseases If your joints hurt, the first thing you should do is find out why they hurt and which joints are affected. Depending on the diagnosis, you may be prescribed a diet. At the same time, there is no universal diet that suits all patients, with damage to any joints, against the background of any diseases of the musculoskeletal system. There are only three diseases for which diet can be an important part of treatment. Let’s arrange them in descending order of importance of proper nutrition: Gout. Osteoarthritis of the hip and knee joints. Rheumatoid arthritis. If you have pulled a ligament, torn a meniscus, developed shoulder arthrosis, adhesive capsulitis, rotator cuff syndrome, or one of the hundreds of other known joint diseases, you don’t need any diet. It won’t cure the disease or even relieve your symptoms. Dietary principles for gout: reducing the consumption of purines and alcohol in order to reduce the level of uric acid in the blood. Nutritional principles for osteoarthritis of large joints of the lower extremities: increasing the consumption of fruits, vegetables, other low-calorie foods, and reducing the consumption of fats and simple sugars to control or reduce body weight. Nutritional principles for rheumatoid arthritis and other autoimmune diseases with joint damage: limiting the consumption of potential allergens and increasing the consumption of beneficial polyunsaturated omega-3 fatty acids. Products that should predominate in the diet In this section we will list the foods that should form the basis of the diet for gout, arthrosis of large joints of the lower extremities and rheumatoid arthritis. Gout The DASH and Mediterranean diets can be the basis of a diet for gout. What you can eat: vegetables; fruits; porridge; vegetable oils; fish; legumes; nuts. It is advisable to include milk and dairy products in the diet. They are useful for such patients, as they improve uric acid metabolism. Yogurt has a particularly beneficial effect on urate metabolism. Previously, soy was limited in gout patients, but now there is evidence that it is safe for gout. Therefore, soy milk, meat and other soy products can be a good replacement for products harmful to joints. Other products that have received “amnesty” and can be part of the diet for gout: citrus fruits, coffee, tea. Osteoarthritis A special diet is required only for those patients who are overweight. In this case, the diet should be dominated by products with low or medium caloric content, with a low glycemic and insulin index. What to eat: vegetables; fruits; whole grain products; legumes; lean meat; dairy products. It is advisable to bake and boil food rather than fry or stew to reduce fat intake. Rheumatoid arthritis The diet can be anything, but with a low content of potential allergens and a high content of omega-3 polyunsaturated fatty acids. They are found in fish, seafood, flaxseed and camelina oil. Omega-3 reduces the risk of rheumatoid arthritis by 35%, and in patients with an existing disease, omega-3 may help with joint pain due to the anti-inflammatory effect. It is worth noting that the effectiveness of omega-3 in this disease has not yet been confirmed by high-quality studies. Products to exclude from the diet In this section we will list foods that should not be eaten if you have gout, osteoarthritis and autoimmune joint diseases. Gout Here’s what you shouldn’t eat if you have gout, so as not to provoke an attack of joint pain: Alcohol. Half of all gout sufferers are people who abuse alcohol. Even occasional drinking increases the frequency and severity of attacks of this disease. Meat and seafood. High consumption of these foods increases the risk of developing gout by one and a half times, and eating them with an established diagnosis increases the frequency of gout attacks by 5 times. Sweet drinks and sugar. Sources of fructose. One serving of a sweet drink per day increases the risk of gout in men by 45%, and two servings by 85%. In women, even one serving increases the likelihood of gout by 74%, two servings by 2.4 times. Osteoarthritis For osteoarthritis of large joints of the legs, it is worth limiting the following products: any confectionery products; bread; mayonnaise; fat meat; salo; smoked sausage; fatty dairy products (sour cream, cream, butter); vegetable oil; nuts and seeds; any other food that is high in fat and high in calories. Limiting such foods will help you lose weight if you are overweight, but it is advisable to combine the diet with exercise. Rheumatoid arthritis An elimination diet can help reduce the severity and frequency of attacks in some patients. It involves limiting foods with high allergenic properties, dyes, and preservatives. It is worth giving preference to natural, ecological food. Some studies show a decrease in blood inflammation markers, pain severity, duration of morning stiffness, and frequency of rheumatoid arthritis attacks when using an elimination diet. Although, in general, the evidence base for diet therapy for this disease
Nutrition and diet for knee arthrosis

Diet plays a minimal role in the treatment and natural clinical course of osteoarthritis. Contrary to overly optimistic publications on the Internet, there is no scientific evidence that eating industrial quantities of jelly, jellied meat, and even animal cartilage can have a beneficial effect on the severity of symptoms or the rate of degradation of articular cartilage. Diet for arthrosis is mainly aimed at reducing or maintaining normal weight in order to avoid excessive stress on diseased joints. What you can’t do with arthrosis With arthrosis, you should not abuse alcohol. It has a negative effect on health in general and on the metabolism of articular cartilage in particular. With arthrosis, you cannot gain weight, and if you have already gained weight, then you should get rid of excess fat on the body. The more you weigh, the greater the load on the knee joints. Accordingly, the faster they deteriorate. It has been proven that weight loss reduces the symptoms of arthrosis, and also increases the period of time before joint replacement, thus having a disease-modifying effect. What you can’t eat with knee arthrosis if you need to lose weight: Any sweets: increase the release of insulin, which causes fat on the sides to grow, and in addition, any confectionery products are high in calories. Fatty meats: pork, beef, etc. Instead: chicken, turkey, rabbit. Fatty sauces such as mayonnaise. Instead: ketchup, soy sauce. Pastries, cakes, pastries. Instead: crackers, fruit jelly, fresh fruits and berries. Other foods rich in fat: butter, vegetable oil in excessive quantities, cheese, smoked sausage, etc. should not be excluded completely, but should be limited. Many people are afraid of low-fat diets, believing that the body needs fats. Indeed, they do. But fats are present in small quantities in almost all foods. Medicine does not know of any diseases that would develop in a person who eats too little fat. But hundreds of diseases are known, the risk of which increases with excessive consumption of fats and sugars. Arthrosis is one of them. The Internet often says that you can’t, but in fact you can: salt, fried, spicy, marinades, soda. Sometimes we see and hear unfounded statements that the listed products accelerate the development of arthrosis by 2-3 times. These data have no scientific evidence and are a product of the authors’ imagination. All the restrictions listed above (fats and sweets) are recommended for people with weight problems. For thin people, this diet does not make sense, since it will not affect the course of arthrosis. What can be done with arthrosis With osteoarthritis of the knee, you can eat everything that does not make you fat. And people gain weight from fatty and sweet foods. Accordingly, you can eat everything that is not fatty and not sweet. Skinny people can eat absolutely everything: even fatty and sweet. But you should give up such food as soon as you notice that your body weight has started to increase. Products that are good for your figure: vegetables; fruits; cereal porridges; whole wheat bread; mushrooms; any unrefined products of plant origin. They write on the Internet that with arthrosis you need to eat a lot of food containing calcium and vitamin D. This is probably due to the similarity of the names of the two diseases: osteoarthrosis and osteoporosis. A lack of vitamin D causes osteoporosis, but not osteoarthrosis. At the same time, there is no doubt that it has a positive effect on bone health. There is evidence that vitamin D improves the ingrowth of endoprostheses into the bone and reduces the risk of repeated endoprosthetics. This vitamin is found in fish, eggs, and is also produced in the skin under the influence of ultraviolet light. Contrary to the myths spread on the Internet, citrus fruits, olive oil, ginger, pineapple, green tea, jellied meat, jelly, offal and fermented milk products do not affect the clinical course of osteoarthritis. Do not rely on these foods, as unfounded diet therapy only distracts from really effective treatment and can cause a delay in seeking medical help. How much water to drink You need to drink just enough water to quench your thirst. In old age, it is worth remembering that the feeling of thirst dulls. You can suffer from dehydration, but still not want to drink. In addition to the feeling of thirst, the fact of dehydration can be determined by dry mouth and dark urine. There is no one norm for everyone, how much to drink. One person weighs 50 kg, another – 100 kg. One lives in a hot climate, another – in a cold one. One runs two hours every day, and the rest of the time works on a construction site, while another lies on the couch and works on the computer. Everyone has different fluid needs. You should drink enough fluid so that your urine is light yellow throughout the day. If it is completely clear, you are drinking too much. If it is darkening, you are not drinking enough. Proper fluid intake is good for your overall health, but it does not affect your joint health. Arthrosis is not treated with water and does not develop as a result of dehydration. If you drink a lot, this does not mean that stage 1 knee arthrosis will never progress to stage 2 arthrosis, or that it will progress more slowly. If you have been diagnosed with arthrosis, you should not rely solely on diet. This is a chronic disease that cannot be cured, but can be controlled. Contact Dr. Waqas Javed’s Clinic in Lahore to get help with arthrosis. To treat this disease, we use not only diet, but also exercise therapy, physiotherapy, intra-articular injections and other methods.
Exercises after knee meniscus surgery

Physical therapy is the most important part of rehabilitation after any operations on the structures of the musculoskeletal system. Although damaged tissues heal on their own, it is important to do exercises to restore muscle strength and range of motion in the joint. The complex is selected individually for each patient. At Dr. Waqas’s Clinic, you can work out with a personal physical therapy instructor. General recommendations before starting training At Dr. Waqas Javed’s Clinic in Lahore, all surgeries for knee meniscus injuries are performed using arthroscopy. Arthroscopy is a minimally invasive technique that involves performing the intervention through several punctures. Therefore, after you have had a partial meniscus removal, recovery will not take long. It will be faster than after other surgeries. In a week or two you will be able to walk without crutches, and in a month and a half you will feel healthy. In three months you will return to the previous functional state that was before the meniscus injury and surgery. The exercise program begins 2-7 days after surgery. This approach varies from clinic to clinic. The time to start training also depends on the patient’s condition and the specifics of the surgery performed. At Dr. Waqas Javed’s Clinic in Lahore, training begins as early as possible, since with this approach to rehabilitation, functional improvements develop faster. Before starting training, it is worth making a program. In our clinic, it is personal for each patient. Rehabilitation is carried out jointly by an orthopedic doctor and a therapeutic exercise instructor. LFK is supplemented by physiotherapy and massage. Before beginning any exercise involving the knee, it is important that most of the swelling has gone down and that the patient is not in severe pain, although some mild discomfort in the operated limb is possible. When choosing exercises, determining the intensity and frequency of training, the general condition of the patient is assessed, the rehabilitation phase is taken into account, as well as the actual condition of the knee joint. What to pay attention to during exercise You should pay attention to your own feelings. If any exercises cause pain or discomfort, tell the instructor about it. At the same time, you shouldn’t be afraid to do exercises even in the first days after surgery. Your knee is not as fragile as you might think. Even if you do something wrong, it doesn’t mean that the tissues inside the knee won’t heal or that you’ll have to have another surgery. Therefore, you should train with sufficient intensity, but at the same time avoid exercises that are not yet acceptable given the rehabilitation phase. For example, it is necessary to choose the right time to add dynamic exercises to isometric exercises, introduce exercises with an expander, with weights, with axial load on the knee joint, etc. An experienced instructor knows which exercises will be useful in a particular period of rehabilitation. Just follow his advice, and the recovery will go smoothly, with good functional results. Exercises in the first 3-7 days after surgery During the first week, you can only walk with support devices such as crutches. Exercises that involve bending the knee joint are not allowed for several days. In the first 3-4 days after the operation, the patient is shown isometric exercises. This means that he tenses the muscles to maintain their tone and improve blood circulation. Examples of such exercises that do not involve the knee joint: A man sits on a bed. He lifts his leg off the floor and moves it 30 cm to the side. Then he returns it to the starting position. Lying on the bed, the person raises the straight leg 15 cm, holds it for 10 seconds, and then lowers it. Since immobilization of the knee joint is not required during the rehabilitation period after meniscus resection, dynamic exercises can be done after 4-5 days, if they do not cause severe discomfort. Examples of such exercises: A person lies on a bed. He bends his leg and pulls his heel towards himself. Over time, this exercise can be made more difficult: not only pull the heel towards you, but also lift it. The man sits on the edge of the bed. He bends his knee and smoothly relaxes the muscles of the thigh. Exercises for 2-4 weeks after surgery From 2-3 weeks, the training possibilities are significantly expanded, as the surgical wounds heal. A person can do the following exercises: Lying on his back, he lifts his leg and rotates it four times. He lowers it and rotates the other leg. He does 10 repetitions on each side. Lying on the stomach, the person bends the legs at the knees and lifts the hip. Lying on his stomach, the patient moves his straight leg back. Lying on your stomach, bring your bent knee to your chest. These are just examples of exercises that are not a complete recovery program. The program can include dozens of types of exercises, and the complex should be selected individually. Exercises for 6-12 weeks after surgery From the sixth week, the functional recovery period begins. You can do almost any exercise, since all the tissues in the knee have already recovered. Now the task is to build up muscles and fully restore joint mobility, if the full range of motion has not yet been achieved. Possible exercises: Lying on his back, a person imitates riding a bicycle. The patient sits on a chair. He makes movements with his legs as if he were swimming breaststroke. A person grasps small objects with his toes and holds them for 5 seconds. You can now do exercises with an expander. It is secured to the lower third of the shin with a loop. The other end is attached to a support. The optimal load (expander resistance level) for most people is medium. Examples of exercises with an expander: A person stands and bends his leg at the knee, touching his heel to his buttock. Bends
Chondromous body in the knee joint, hip, shoulder joint – removal, surgery

A chondromous body is a free fragment of cartilaginous and/or bone tissue that can be fixed to the joint capsule or freely “dangle” inside the joint cavity. Chondromous bodies can be single or multiple. They can appear anywhere: in the hip, in the shoulder joint, but are most often found in the knee joint. It is important to promptly remove the bone-cartilaginous fragments to avoid irreversible damage to the articular cartilage. Symptoms knee pain; it is impossible to fully straighten the leg; knee flexion is blocked; crunching when moving; palpable dense formations under the skin. Treatment minimally invasive arthroscopic surgery; evacuation of chondromal bodies; partial synovectomy; mosaic autochondroplasty; rehabilitation 6 weeks. Our advantages we perform operations using minimally invasive arthroscopic methods; adequate intraoperative and postoperative pain relief; we successfully extract even large chondromal bodies; we restore damaged tissues of the knee joint; We provide complete rehabilitation. Causes of the appearance of chondromal body in joints Free intra-articular bodies in the knee can be represented by a wide variety of tissues: these are not only cartilaginous and bone fragments, but also “fragments” of torn menisci, ligament fragments, fibrous (compacted) villi of the synovial membrane. After unsuccessful knee surgeries, fragments of bone cement, staples and screws can “travel” inside the joint. But most often, the torn fragment is a piece of patellar cartilage. If it consists only of cartilaginous tissue, without bone tissue, then it is not displayed on X-rays. Therefore, if you have an X-ray and there are no signs of pathology, this does not mean that chondromal bodies are absent. They can be detected using MRI. Single chondromalacia patellae may appear in various diseases: chondromalacia of the patella, patellofemoral arthrosis, trauma, Koenig’s disease (death of a fragment of cartilage and bone in the knee). Cartilaginous bodies can have a wide variety of sizes and shapes. Small fragments are those up to 3 mm in the largest dimension, medium – up to 1 cm, large – from 1 cm. Free chondromal bodies constantly move within the joint, and if they reach large sizes, they can be contoured and palpated by the patient. During surgery, they can be difficult to find and remove. These cartilage fragments constantly try to slip out and “escape”. Therefore, they are informally called “joint mice” The main problems caused by these “animals” are: constant irritation of the synovial membrane; pain in the knee; wedging between the articular surfaces with the inability to straighten or bend the leg; periodically occurring synovitis (inflammatory processes of the synovial membrane) with swelling, redness, and accumulation of fluid in the knee; In the long term, osteoarthritis may develop due to damage and adverse effects on the metabolism of articular cartilage. A rare cause of the formation of chondromal bodies, often multiple, is primary synovial chondromatosis. In this disease, the cartilaginous bodies do not break away from the normal cartilage, but grow directly on the synovial membrane. Then some separate and become “joint mice”, while others remain fixed, but can gradually increase in size and reach impressive sizes. In standard cases, 10 to 20 cartilaginous bodies are formed in a short period of time, and then they do not increase in size or quantity. But in severe cases, new bone-cartilaginous bodies are constantly formed, grow continuously, and in such a situation, the only way to solve the problem is to completely remove the synovial membrane of the knee joint. There are also forms of the disease in which the cartilaginous bodies grow together, forming giant conglomerates. They occupy most of the joint cavity, making the joint practically immobile. How does the removal operation work? An operation to remove the chondromal body is the only way to solve the problem. It will not go away or dissolve on its own. If the chondromal body remains in the joint cavity for a long time, it will gradually damage the synovial membrane and articular cartilage, causing irreversible pathological changes. As a result, chondromal bodies can destroy your joint. To prevent this from happening, seek help in a timely manner. The operation to remove the chondromal body is performed using a minimally invasive arthroscopic method. In uncomplicated cases, this intervention does not take much time, is not associated with major trauma, and recovery is very fast. How the operation is performed: Pain relief: spinal anesthesia or general anesthesia. Making several incisions up to 0.5 cm in the knee joint area. Installation of cannulas (expanders) that allow the removal of chondromal bodies. Insertion of an arthroscope and examination of the knee joint to identify all chondral bodies and assess the condition of intra-articular tissues (menisci, articular cartilage, synovial membrane). Extraction of chondromal bodies entirely or with preliminary fragmentation. A possible stage of the operation is partial synovectomy – partial removal of the synovial membrane if it is damaged and inflamed. It happens that chondromous bodies elude the doctor, and he cannot grasp them to pull them out. In this case, an additional puncture with a needle may be required to fix the fragment, or the installation of an additional port for the introduction of a clamp with a serrated working surface. Although very large chondromal bodies must be fragmented, doctors still try to avoid this procedure by removing them whole. This may require making a slightly larger incision than usual. Some cartilaginous bodies are fused with the synovial membrane. In this case, they are first captured so that the joint mice do not escape after separation, and then cut off from the synovial membrane with an electric knife. Sometimes it is necessary to restore the defect of the articular cartilage in the place where the fragment “fell off”. Mosaic autochondroplasty can be used for this purpose. The doctor takes fragments of cartilage from the non-load-bearing area of the knee joint to install them in the defect area. Although this procedure significantly increases the rehabilitation period, it prevents the development of osteoarthritis of the knee joints. Rehabilitation after surgery If the operation to remove chondromal bodies was performed
Knee replacement: what you need to know?

Knee joint endoprosthetics is an effective and often the only way to restore lost limb function. Total, i.e. replacement of all joint components, endoprosthetics is the method of choice in the treatment of: degenerative-dystrophic diseases (arthrosis-arthritis) rheumatoid polyarthritis post-traumatic arthrosis malunion of intra-articular fractures of one or both articular surfaces bones that make up the knee joint damaged ligamentous apparatus of the knee joint with pronounced changes in the articular ends of bones What should a patient know about endoprosthetic surgery? This is a very precise surgical intervention, the purpose of which is to return you to a mobile, painless joint, allowing you to return to your normal life. The development of technical progress has led to the emergence of materials that can replace a worn-out joint with an artificial one. Just like a regular knee joint, an artificial one precisely replicates the elements of a normal joint, allowing the necessary range of motion. Implantation of an artificial knee joint does not require extensive bone resection and the operation preserves the knee joint’s own ligamentous apparatus, except in cases where the ligamentous apparatus is damaged and requires its restoration. An appropriate prosthesis is selected for each specific case. Consultation During the consultation, the doctor will determine the indications and contraindications for joint endoprosthetics, conduct the necessary examinations and select the appropriate prosthesis. An X-ray examination will help determine the degree of joint wear and tear and make the necessary measurements. You will be warned about the possible risks and complications of the operation. The following may be considered complications of the operation: infection in the surgical area bleeding during or after surgery thromboembolism (blockage of a vessel by a blood clot) Before the operation Before the operation, the patient undergoes a full clinical examination (tests, specialist consultations, anesthesiologist examination). The patient is hospitalized 1-2 days before the operation. Operation In standard cases, implantation of an artificial joint lasts 2-3 hours. During the operation, measures are taken to prevent infectious complications, if necessary, to replenish blood loss, and to drain the wound to prevent blood accumulation. After operation In the postoperative period, the administration of antibiotics, painkillers, and symptomatic treatment continues. Inpatient rehabilitation treatment Activation in bed is permitted as early as the first day after surgery. From the second day, you can sit up in bed, start static exercises for the limb muscles, and do breathing exercises. Walking with a measured load on the operated limb and additional support (crutches, playpen) is possible as early as the third day. The stitches are removed on the 10th-12th day. Discharge home Discharge is made 10-12 days after the operation. It is necessary to continue rehabilitation measures, strictly following the recommendations of the operating surgeon. If necessary, hospitalization in a rehabilitation center for recovery under the supervision of specialists – rehabilitation specialists is possible. Restrictions on physical activity on the operated limb should be observed for 6 weeks after the operation, during this time it is recommended to use additional support.
Hip replacement: what you need to know?
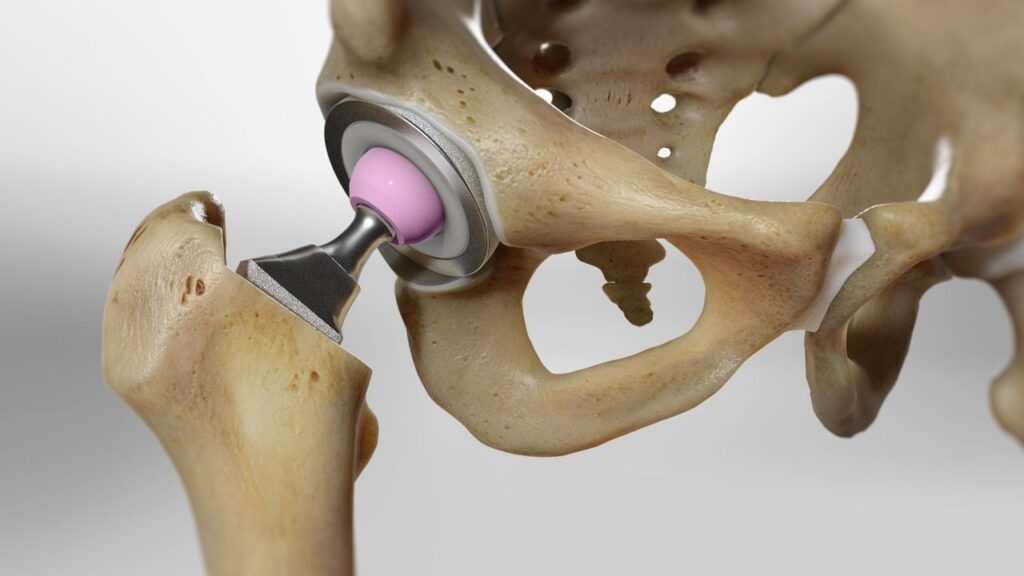
Hip replacement is an effective and often the only way to restore lost limb function. Total, i.e. with replacement of all components of the joint, endoprosthetics is the method of choice in the treatment of: Bechterew’s disease (with predominant damage to the hip joints) degenerative-dystrophic diseases (arthrosis-arthritis) rheumatoid polyarthritis aseptic necrosis of the femoral head pseudoarthrosis of the femoral neck and non-union of femoral neck fractures What should a patient know about endoprosthetic surgery? This is a very precise surgical intervention, the purpose of which is to return you to a mobile, painless joint, allowing you to return to your normal life. The development of technical progress has led to the emergence of materials that can replace a worn-out joint with an artificial one. Just like a normal hip joint, an artificial one consists of a round head and a concave socket in which the head rotates, allowing for a normal range of motion. For each specific case, an appropriate prosthesis is selected. Consultation During the consultation, the doctor will determine the indications and contraindications for hip replacement, conduct the necessary examinations and select the appropriate prosthesis. An X-ray examination will help determine the degree of wear of the joint and make the necessary measurements. You will definitely be warned about the possible risks and complications of the operation. The following complications may be considered: infection in the surgical area bleeding during or after surgery thromboembolism (blockage of a vessel by a blood clot) development of pneumonia dislocation of the prosthesis, which will require an increase in the treatment period Before the operation Before the operation, the patient undergoes a full clinical examination (tests, specialist consultations, anesthesiologist examination). The patient is hospitalized 1-2 days before the operation. Operation Hip replacement is a complex surgical intervention that requires high professionalism of the surgeon. In standard cases, implantation of an artificial joint lasts 2-3 hours. During the operation, measures are taken to prevent infectious complications, if necessary, to replenish blood loss, and to drain the wound to prevent blood accumulation. After operation In the postoperative period, antibiotics, painkillers, and symptomatic treatment continue. A bolster is placed between the legs to hold the operated limb in the correct position. Inpatient rehabilitation Activation in bed is permitted as early as the first day after surgery. From the second day, you can sit up in bed, start static exercises for the limb muscles, and do breathing exercises. Walking with a measured load on the operated limb and additional support (crutches, arena) is possible as early as the third day. The stitches are removed on the 10th-12th day. Discharge home Discharge is made 10-12 days after the operation. It is necessary to continue rehabilitation measures, strictly following the recommendations of the operating surgeon. If necessary, hospitalization in a rehabilitation center for recovery under the supervision of rehabilitation specialists is possible. Restrictions on physical activity on the operated limb should be observed for 6-8 weeks after the operation, during this time it is recommended to use additional support.
Achilles tendon injuries

The most powerful and largest tendon of a person is located in the back of the leg, is formed as a result of the fusion of flat tendons of the gastrocnemius and soleus muscles and is attached to the tuberosity of the calcaneus, and is called the Achilles (heel) tendon . It is responsible for the movement of the foot (flexion-extension), for the ability of a person to walk upright, and also performs a shock-absorbing function. But, despite its strength and durability, it is injured quite often. The risk group most often includes athletes (runners, jumpers, gymnasts), circus performers, professional dancers, but in everyday life, injuries to the Achilles tendon are also common (slipping of the foot from a curb or step, twisting of the foot when walking in high heels – in women, etc.) Types of injuries Tendinitis is an inflammatory disease of the tendons, in which microtraumas are observed that do not violate the integrity of the tendon itself. Stretching Tendon ruptures (partial or complete) The causes of trauma are: direct injuries to the tendon area (kicks or sharp object blows (open injuries); sudden sharp load on the foot area without prior preparation (sharp start, unsuccessful jump, etc.); biochemical factors (flat feet, high arches, bowed legs, etc.); existing inflammatory processes in the heel area (bursitis, tendovaginitis); age over 40 years (ligament extensibility decreases, which leads to increased trauma); wearing uncomfortable shoes (high heels, narrow toes, hard backs); chronic diseases (osteoarthritis, rheumatoid arthritis , gout ); obesity Symptoms: acute intense pain in the area of injury swelling, followed by bruising when it breaks, a characteristic crunch or cracking sound is heard with tendonitis – creaking it is impossible to bend the foot, attempts to do so cause sharp pain, and it is also impossible to stand on the foot and stretch the foot a depression or notch appears at the site of the damaged Achilles tendon A qualified specialist will help diagnose the presence of an injury by conducting a thorough examination of the damaged area and analyzing the patient’s complaints. In complex cases, the doctor may refer the patient for an X-ray, ultrasound, or MRI. If you suspect that you have an Achilles tendon injury, you should be examined by the following specialists : traumatologist-orthopedist surgeon rheumatologist Treatment and recovery In case of serious injuries (for example, an open tendon rupture), the victim requires urgent hospitalization. In the traumatology department, the patient will undergo surgery, during which the torn tendons are sutured and subsequent rehabilitation treatment is performed. In case of other types of injuries (tendinitis, sprains, partial ligament rupture), the patient undergoes conservative treatment, which includes: drug therapy (taking anti-inflammatory and pain-relieving medications) cryotherapy reducing or eliminating the load on the injured limb. To ensure immobility, splints, plaster casts, bandages, orthoses (brace) are used physiotherapy treatment physiotherapy exercises, which are prescribed after the Achilles tendon has healed massage. During the rehabilitation period, it is recommended to avoid heavy physical activity and wear and select comfortable shoes.
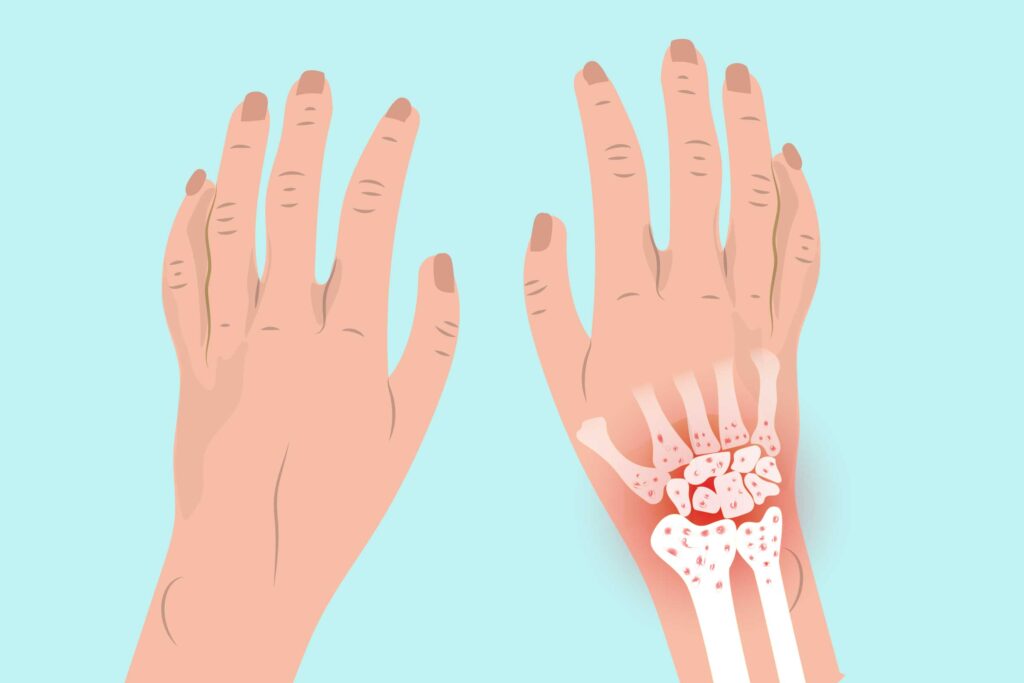
Rheumatoid arthritis of the hands

Rheumatoid arthritis is a systemic disease of connective tissue with predominant damage to small joints. Rheumatoid arthritis can start in any joint, but most often begins in the small joints of the fingers, hands, and wrists. Joint damage is usually symmetrical, meaning if a joint on the right hand hurts, the same joint on the left is most likely to hurt. Symptoms to look out for Fatigue; Morning stiffness; Weakness; Flu-like symptoms; Pain when sitting for a long time; Outbreaks of disease activity accompanied by remission; Muscle pain; Loss of appetite, depression, weight loss, anemia, cold and/or sweaty palms and feet; A disorder of the glands around the eyes and mouth that causes insufficient production of tears and saliva. There are 3 main factors that are identified as the cause of the disease (rheumatological triad) Genetic predisposition Hereditary predisposition to autoimmune reactions More common in carriers of a certain MHC class II antigen: HLA – DR1, DR4 Infectious factor paramyxoviruses – viruses of mumps, measles, respiratory syncytial infection hepatoviruses – hepatitis B virus herpesviruses – herpes simplex viruses, herpes zoster, cytomegalovirus, Epstein-Barr virus retroviruses – T-lymphotropic virus Trigger factor (hypothermia, hyperinsolation, intoxication, mutagenic drugs, endocrinopathies, stress, etc.) . For women, the duration of breastfeeding reduces the likelihood of developing RA. Breastfeeding for 24 months or longer reduces the risk of developing RA by half. Diagnosis of the disease It is based on a biochemical blood test , changes in the joints visible on an X-ray , and the use of basic clinical markers . Blood tests examine ESR, rheumatoid factor, platelet count, etc. The most advanced test is the titer of antibodies to cyclic citrulline-containing peptide – anti-CCP, anti -CCP . The specificity of this indicator is about 90%, while it is present in 79% of sera from patients with RA. Diagnostically important clinical features include the absence of changes in skin color over inflamed joints, the development of tendosynovitis of the flexors or extensors of the fingers of the hands, and the formation of amyotrophy, typical deformations of the hands, the so-called “rheumatoid hand”. The criteria for an unfavorable prognosis are: early damage to large joints and the appearance of rheumatoid nodules; enlarged lymph nodes; involvement of new joints during subsequent exacerbation; systemic nature of the disease; persistent increase in ESR; early onset (within the first year) and high titers of rheumatoid factor; early (up to four months) radiological changes in the affected joints – rapid progression of destructive changes; detection of antinuclear antibodies and LE cells; carriage of HLA-DR4 antigens; poor tolerance of basic drugs. In the treatment of rheumatoid arthritis, systemic drug therapy with various groups of drugs is used.
Arthrosis and osteoarthrosis of the wrist joint
The wrist joint is one of the most important elements of the musculoskeletal system of the human body. This fragile joint is located at the junction of the hands and forearm bones. Most often, this area is subject to injuries, degenerative changes are much less common here. Arthrosis of the wrist joint is a rather rare disease and can greatly reduce a person’s quality of life. Constant loads and injuries provoke degradation of cartilage tissue, which is subsequently accompanied by pain and difficulty in movement. This is how osteoarthritis of the wrist joint develops , causing serious discomfort. Joint mobility is sometimes reduced by half, which causes severe discomfort in the process of performing everyday, habitual manipulations. Symptoms of arthrosis and osteoarthrosis It is difficult to recognize these diseases at the initial stages. Patients often do not pay attention to mild pain, and when it becomes strong enough, the disease is already advanced. Pain when moving, causing discomfort and serious inconvenience in everyday activities. This is one of the most characteristic symptoms of arthrosis and osteoarthrosis of the wrist joint. Pain when trying to lean on the palm, bending the wrist, carrying heavy objects. In some cases, edema occurs, and swelling appears in the areas affected by the disease. Joint crunching, feeling of limited movement. Types and degrees of diseases Arthrosis and osteoarthrosis of the 1st degree have not very pronounced symptoms and are manifested by minor pain after loads, especially monotonous ones. As soon as the joints return to a state of rest, the pain disappears. The development of stage 2 of the disease is accompanied by the appearance of more pronounced problems – pain and discomfort that do not go away for a long time. There is a crunch in the joints, swelling in the phalanges. The patient tries not to make painful movements. The third stage is manifested by increased deformations, the appearance of deforming osteoarthrosis, pain at rest, and limited movement. At this stage, the cartilaginous layer is almost completely destroyed, and bone growths may appear along the edges of the joints. Due to decreased motor activity, the muscle tone of the entire arm decreases. Which doctor should I see? It is insidious and develops almost without symptoms until it reaches a serious stage. For example, deforming arthrosis can develop as a result of an injury (post-traumatic arthrosis) and not make itself known until serious, difficult-to-treat changes appear. You can contact a therapist, describe the problem and get a referral, or immediately visit a rheumatologist. A dermatologist, urologist, and other specialized doctors can also be involved in solving the problem. Diagnostics To make an accurate diagnosis, which is extremely important for successful treatment, a set of diagnostic measures is needed: Examination and questioning of the patient at an appointment with an orthopedist. Palpation. X-ray in two or three projections depending on the clinical picture. General tests. Ultrasound, CT or MRI if necessary. Consultation with other specialists if necessary. Causes of occurrence Osteoarthritis can be primary – developing in a healthy joint, or secondary – developing in a joint that has already been affected by some disease. The factors that contribute to the development of deforming osteoarthritis are the following: Gender – women are much more susceptible to developing arthrosis of the joints. Age-related – after 65 years of age, almost 90% of people have joint pathologies. Excess weight, endocrine disorders. Excessive strain on the wrist joint. Heavy physical work, professional sports. Advanced inflammatory processes in the joints. Heredity. Treatment In each case, the approach to how to treat the disease may be different. It depends on the degree of the disease, the causes that caused it, the patient’s condition, the damage to the right or left wrist. Among the main methods: Exercises, special therapeutic gymnastics. Physiotherapy. Treatment with medication. Maintaining proper nutrition and daily routine. Wearing chondroprotectors that help the process of cartilage tissue restoration. Taking medications and injections to help restore cartilage. When the disease reaches an advanced stage, the only way to help the patient is through surgery and prosthetics. It is important to understand that this disease is chronic, which means that treatment procedures will have to be carried out constantly. However, the earlier osteoarthritis of the wrist joint is diagnosed, the more timely the therapy will begin and the destructive changes in the cartilage tissue will be less. This determines the importance of contacting an orthopedist at the slightest signs of pathology in the joint area. Recovery Recovery is aimed at returning motor activity and joint functions. Rehabilitation mainly consists of performing gymnastics, therapeutic exercises, and establishing a balanced nutrition system. Wearing fixing bandages and dressings to speed up the restoration of cartilaginous tissue also gives good results. To prevent deforming osteoarthritis and other similar diseases – maintain normal body weight, avoid heavy loads, pay close attention to changes in health.